

Chemotherapy: how to prevent and relieve mouth ulcers and mucositis?

In order to beat cancer, I, like many of you, underwent a chemotherapy protocol and endured its share of side effects.
Mouth lesions, such as canker sores, gingivitis, mucositis and dryness are frequent side effects that I unfortunately did not escape.
How to forget that unpleasant feeling of eating rusty nails.
In this article, I will give you some information that I hope will be useful to prevent and/or relieve your oral lesions.
Dry mouth, mouth ulcers and mucositis
An adverse effect of cancer treatments
The cytotoxic action (directed against cells) of anticancer treatments is mainly exerted against rapidly dividing cells. This is the case for cancer cells but also for “healthy” cells in the body and in particular for epithelial cells. The latter cover the walls of the oral cavity (palate, gums, tongue, floor of the mouth, inner cheeks, lips). Chemotherapy and radiotherapy induce a modification in the renewal of these cells, which contributes in altering the integrity of the mucous membranes of the mouth and can lead to lesions.
Dry Mouth
Treatments can also contribute to a decrease in saliva and consequently to dry mouth.
Saliva has a protective and immune role for the different cells in the mouth. Its decrease, associated with a decrease in the body’s defenses, increases the risk of bacterial and fungal infections. In addition, a dry and ulcerated mouth is at risk of bleeding, especially since the number of platelets in the blood is often reduced by chemotherapy.
You may experience different symptoms (or none at all): dry mouth, ” pasty ” mouth, bad breath, change in the consistency of saliva, difficulty or pain when chewing food, pain or sore throat, difficulty swallowing, swelling, redness, ” raw ” gums, tingling or burning, gum wounds, a feeling of discomfort (lump in the throat) or pain when swallowing, ulceration(s) in the form of erosions or mouth ulcers.
Mouth ulcers and mucositis
 Mucositis is an inflammation of the mucous membrane that lines the interior of cavities and viscera. It is due to the alteration of the epithelium and the underlying connective tissue, causing ulcerations. This can lead to the development of ulcers (canker sores). Mucositis can also affect the esophagus and be similar to a sore throat. The discomfort and pain caused by these ulcers can lead to less food being eaten and therefore to weight loss and/or undernutrition. Mucositis may appear during the first week of treatment. They then gradually resolve during the following week, with a risk of recurrence if treatment is continued. (new chemotherapy or radiotherapy session)
Mucositis is an inflammation of the mucous membrane that lines the interior of cavities and viscera. It is due to the alteration of the epithelium and the underlying connective tissue, causing ulcerations. This can lead to the development of ulcers (canker sores). Mucositis can also affect the esophagus and be similar to a sore throat. The discomfort and pain caused by these ulcers can lead to less food being eaten and therefore to weight loss and/or undernutrition. Mucositis may appear during the first week of treatment. They then gradually resolve during the following week, with a risk of recurrence if treatment is continued. (new chemotherapy or radiotherapy session)
Preventing mucositis
To date, the treatment of mucositis relies mainly on supportive care. Prevention is therefore essential and oral hygiene is the key.
Good oral hygiene
Before starting your treatments, it is advisable to consult a dentist in order to treat any dental problems that may be present.
Here are some practical tips to prevent the risk of mouth lesions:
• Brush your teeth gently after each meal, using a very soft brush to avoid damaging the gums, and rinse well after each use.
•Avoid trauma: preferably no electric toothbrushes, toothpicks or dental floss.
 • Use a gentle, non-abrasive, menthol-free toothpaste. Ozalys mild toothpaste, Essential Care, (link) has been specifically designed to bring you softness, freshness and comfort.
• Use a gentle, non-abrasive, menthol-free toothpaste. Ozalys mild toothpaste, Essential Care, (link) has been specifically designed to bring you softness, freshness and comfort.
•Rinse your mouth thoroughly, as often as possible.
•Do not use mouthwash containing alcohol. Our mouthwash, Comfort Care, soothes and refreshes, bringing comfort to your mouth.
•Moisturize your mouth by sucking on ice cubes or candy to stimulate salivary secretion.
•Moisturize your lips with a lip balm or simply with Vaseline.
•If you have a denture, remove it and clean it after each meal in an antiseptic effervescent solution, renewed every day. If your apparatus does not fit properly or irritates your mouth and gums, it is best not to use it.
An adapted diet
Various dietary measures are recommended to prevent the onset of mucositis:
• Keep yourself sufficiently hydrated (on average 2 liters/day) by varying the intake of beverages at your convenience. Avoid coffee and prefer green tea-based drinks. You can also spray your mouth with pure water sprays.
•Eat light, frequent meals rather than large ones. Food should be slightly warm or at room temperature, and hot dishes and drinks should be avoided.
•Prefer liquids and soft or blended foods and favor cold, room temperature or iced foods: ice creams, mashed or pureed cooked vegetables, mashed or blended meats or fish.
• Avoid hard or crunchy foods (hazelnuts, potato chips…), acidic foods such as citrus fruits, tomatoes, grapes, apples, strawberries, vinegar, mustard. Also avoid spices, pepper and chilli, fried and/or salty foods (cookies, peanuts…), irritating foods (gruyere cheese, nuts, pineapple…).
•Avoid as much as possible alcohol and tobacco, irritating, acidic, hard, spicy foods and nuts (walnuts, almonds, hazelnuts, peanuts).
The management of mucositis
Measuring the severity of mucositis
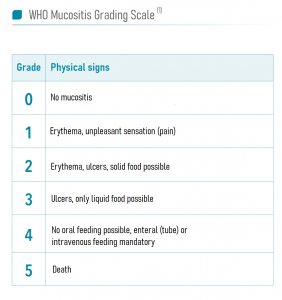 The severity of oral-pharyngeal mucositis is assessed with the WHO classification scale. Mucositis is classified in 4 grades.
The severity of oral-pharyngeal mucositis is assessed with the WHO classification scale. Mucositis is classified in 4 grades.
In the first grade, there is a slight discomfort at mealtime.
In the second grade, painful mouth ulcers appear.
In grade 3, the mucosa is eroded and one ingests only liquid food.
At grade 4, the pain is so bad that one cannot swallow anymore. In this case, it is necessary to be fed through a tube.
Rest assured, extremely serious cases are rare.
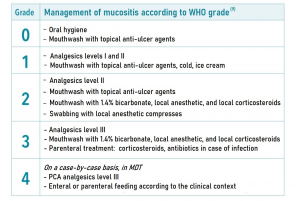 To date, the general recommendations for the management of mucositis are mainly based on oral hygiene and the use of mouthwashes.
To date, the general recommendations for the management of mucositis are mainly based on oral hygiene and the use of mouthwashes.
Specific treatments are often prescribed by your doctor depending on the severity of the mucositis. Local or general analgesic or anesthetic treatments can also be used.
Some tips to relieve mucositis
•In case of mucositis, certain dietary measures are recommended to limit the discomfort and pain caused by the ulcerations. Put into practice the recommendations indicated above concerning prevention, by favouring a “non-irritating” diet.
Do not hesitate to abuse ice cubes, crushed ice, water ice, sorbets and mints (candy).
A little tip: use a straw to prevent drinks from coming into direct contact with damaged mucous membranes.
If you have difficulty eating, you can be offered additional care: for example, enriched nutritional preparations that are easy to swallow or, if necessary, the temporary placement of a feeding tube.
•Discuss with your doctor the possibilities of pain treatment: gels for local application or medication. If they are too painful to take, they can be prescribed in the form of syrups, suppositories or injections (for temporary use).
Advances and innovations…Weaving light to treat mucositis
Today, the effectiveness of photo-biomodulation is well established. Also known as low-energy laser therapy, it uses light energy to elicit biological responses from the cell and normalize cell function. In fact, it entered international guidelines in July 2019 as the primary first-line treatment for mucositis. Yet few patients benefit because the method is complex to implement. “We have laser pens but you have to treat the injured area point by point. It is long and difficult, so few doctors use them,” explains Professor René-Jean Bensadoun. (Oncologist-Radiotherapist, High Energy Center, Nice).
NeoMedLight, which develops innovative medical devices designed for phototherapy, is proposing a new light-based treatment for mucositis. Neomedlight has developed a light-based textile that overcomes the limitations of current biomodulation devices. “With this fabric, we can treat a larger area of skin at once. And since we are in contact with the skin, there is no longer this problem of distance. The weave also ensures a homogeneous dose over the entire treated area,” acknowledges Prof. Bensadoun.
Another important advantage is the duration of the treatment. Where the laser pen required 30 to 45 minutes of handling, the Neomedlight fabric only requires about 10 minutes.
If you want more information, I invite you to visit their website https://www.neomedlight.com/fr/photobiomodulation/
In conclusion
Oral lesions are common side effects reported by patients undergoing chemotherapy and/or radiotherapy. The discomfort caused and the pain induced have negative consequences on the quality of life: restricted diet, weight loss … Sometimes, they even have an impact on the implementation of the treatment (reduction or spacing of doses) to the point of demoralizing the people concerned.
Because the management of these lesions is still essentially based on prevention, thanks to 3 years of research and a mobilized R&D team, the Ozalys Laboratory offers a toothpaste and a mouthwash specially designed to help you take care of your weakened mouth.
Because in this battle for life, comfort and reassurance are so precious.

