

Breast Cancer, Numbers and Letters…

“Pink October”, is breast cancer awareness month, which is dedicated to the prevention and control of breast cancer.
Because more than 2 million women around the world face this terrible diagnosis every year and its early onset has a direct impact on their chances of survival, the month of October is essential worldwide.
This fight, which affects nearly 1 in 8 women in France, is not limited to defeating the disease. After the acute phase of treatment, prevention of recurrence is omnipresent.
Another period of life to be assumed and built up.
The specifics of breast cancer patients management
TNM…Not one, but breast cancers
pT2N1, GIII, RH+, HER2- behind this example of a long series of Numbers and Letters lies the cancer number, an identity card that determines the protocol of care.
The TNM classification is an international standard code, proposed in 1959 by the American Joint Committee on Cancer, which allows cancer teams to identify the stage of a cancer. (link e-cancer website)
The letter T (Tumor): followed by a number from 0 to 4 describes the size of the tumor and its extension to the skin or chest wall below the breast. T4 tumors are the largest and extend to the tissue surrounding the breast gland.
The letter N (Node): followed by a number from 0 to 3 indicates whether the cancer has spread to the lymph nodes near the breast under the armpit.
The letter M (Metastasis): followed by a 0 or a 1 indicates whether or not the cancer has spread to distant organs.
Depending on the type of cancer, different treatments are offered to remove the tumour, slow the development of the disease or reduce the risk of recurrence: surgery, chemotherapy, radiotherapy, hormone therapy and targeted therapies.
If you want to understand everything about breast cancer, I invite you to download for free the books of Dr. Elia, gynecologist: http://docteurdavidelia.fr/internet/index.php?numrubrique=166&numsousrubrique=379
RH+… 80% hormone-sensitive breast cancer
Hormones, are a substance secreted in the blood by certain tissues or glands of the human body, which transmit a message to organs located at a distance. To decode this message, the organs must be equipped with sensors called receptors.
 “The hormone can be compared to a “sophisticated key” and its receptor to a “high-security lock”: when the key “fits” well into its specific lock, it causes a precise biological action. The nuclei of healthy breast cells are equipped with these receptors. The hormones estrogen and progesterone, by penetrating these receptors, ensure their proper development. The search for the maintenance or not of the hormonal receptors in the nuclei of the cancerous breast cell is essential to evaluate the prognosis: the tumor is then often less aggressive and less likely to spread.”
“The hormone can be compared to a “sophisticated key” and its receptor to a “high-security lock”: when the key “fits” well into its specific lock, it causes a precise biological action. The nuclei of healthy breast cells are equipped with these receptors. The hormones estrogen and progesterone, by penetrating these receptors, ensure their proper development. The search for the maintenance or not of the hormonal receptors in the nuclei of the cancerous breast cell is essential to evaluate the prognosis: the tumor is then often less aggressive and less likely to spread.”
It is the pathological examination of the cells under the microscope that determines whether or not they have hormone receptors (HR). RH+ or -, this sign alone will determine whether or not you can be offered hormone therapy.
To date, 80% of breast cancers are hormone-sensitive (or hormone-dependent).
M … Metastatic cancer
M…behind this letter are metastases and an indefinite course of care.
20 to 30% of patients diagnosed with breast cancer will develop metastases early or during the course of their disease.
This is an advanced form of the disease. It is called metastatic or stage 4 cancer, when cancer cells are no longer located only in the breast and local lymph nodes, but have spread to other parts of the body, most often to the bones, liver, brain or lungs.
Because metastatic breast cancer must not be forgotten, I wish to support and highlight the commitment of the 1310 collective.
Preventing breast cancer from recurring.
Breast cancer is the most common female cancer in Western countries and the second leading cause of death in women.
The prognosis depends on various factors, including the stage and type of breast cancer. Another 12,000 women die each year in France, the vast majority of them in the event of a recurrence.
Approximately 75% of recurrences occur within 5 years of diagnosis, but it remains difficult to find accessible figures on this subject. Why is it difficult to find accessible figures on this subject? Is it a taboo? What proportion of the 12,000 deaths each year is attributable to relapses?
An indispensable regular follow-up
For those around us, the end of the treatment marks the beginning of a new life.
The words are meant to be benevolent: “You have to turn the page: it’s over, move on. “The reality is quite different. After the acute phase of treatment, regular and prolonged follow-up is essential to avoid a recurrence or to detect it as early as possible.
The frequency of follow-up is individualized and will depend on the risks and impact of cancer treatment on each of us.
How can we act “as if nothing had happened”, when these regular check-ups remind us that we have been sick, that each medical examination is a source of anxiety? How can we live with this sword of Damocles hanging over our heads? How can we forget, when medical check-ups will punctuate our agendas until the end of our lives.
No, nothing will ever be the same again, the experience of the disease marks us forever and the fear of recurrence is omnipresent.
This year 2020 is all the more anxiety-provoking. More than cancer, it is a pandemic that has been at the center of attention for months: covid-19. Dramatic in itself, this virus has a cascading effect on the screening, diagnosis, treatment and follow-up of breast cancer. According to Rose-Up: “this year, the covid-19 epidemic is discouraging many French women from having their mammography exams, which are considered ‘secondary’. Oncologists are alarmed: tumors not detected in time cause thousands of additional deaths”.
In the particular case of genetic mutations
The prognosis for breast (and ovarian) cancer depends largely on the early treatment, not on the presence of a genetic mutation. However, cancers favored by a BRCA mutation are often the most aggressive.
Deleterious BRCA mutations increase the risk of recurrence. For this reason, treatment options are different from those offered to a person who does not carry a gene mutation.
Risk reduction surgery may be indicated: mastectomy and/or preventive ovarian surgery.
For more information on this subject, I invite you to consult the Geneticancer Association website.
Hormone therapy…what a funny name!
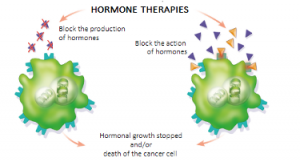
Contrary to what its name might suggest, hormone therapy is not a hormone-based treatment. On the contrary, its aim is to block the action of hormones and thus avoid “feeding” the cancerous tumors.
It can be used in neoadjuvant treatment (prior to surgery) to reduce the size of the tumor and make it operable, and/or in adjuvant treatment to help reduce the risk of recurrence. It is intended only for affected women whose tumor is hormone-sensitive (RH+).
There are 3 types of hormone therapy. All three have the same goal: to prevent hormones from producing their normal actions of stimulating breast cells.
- Anti-estrogens prevent estrogens from binding to their receptors and thus interfere with the delivery of their message to stimulate tumor cell growth. They are often prescribed to non-menopausal women or as a second line of treatment, for example in cases of intolerance to anti aromatase inhibitors.
- Anti-aromatase or aromatase inhibitors. Aromatase is an enzyme that allows the continued production of estrogen by the transformation of male hormones after menopause. These drugs compete with “aromatase” and prevent it from working.
- LH-RH analogues. These drugs induce an “artificial” menopause and therefore oppose the production of hormones by the ovaries.
This treatment is usually prescribed as an adjuvant for at least 5 years. While this treatment significantly reduces the relapse and mortality rates, recent studies (study link) have shown that an extension would further reduce the risk of recurrence, so the administration time tends to be longer than 10 years.
There is also a non-drug treatment, which consists of stopping the production of estrogen by the ovaries by removing it surgically (oophorectomy) or by irradiating it (radiotherapy).
Hormone therapy can be accompanied by a number of undesirable effects that can sometimes significantly affect our quality of life. It is a kind of “menopause to the power of 1000”: weight gain, hair loss, muscle and joint pain, fatigue, migraines, hot flashes, vaginal dryness, loss of libido… The list is long and the side effects are sometimes so heavy that they frequently lead to treatment abandonment.
Protect yourself from hormonal sources
Hormone therapy, however heavy it may be to bear, allows, by neutralizing them, to protect us from endogenous hormones, likely to feed the cancerous tumor.
Since the objective for hormone-sensitive cancers is to neutralize hormonal sources, we should not introduce new exogenous ones.
Dr. Elia’s opinion: “These hormones look like natural hormones but are not. They can therefore sometimes lure the hormone receptors, which then receive the “false hormones” as a natural hormone with the dangerous consequences of disrupting the functioning of the cells: once the “Trojan horse” enters the place, a lot of serious damage can occur.”

Phthalate, parabens, soy, sage, aluminum, alum stone.. these names may not mean anything to you, but they are part of our daily environment. From the bathroom, to the kitchen, to packaging, these endocrine disruptors surround us.
According to the World Health Organization (WHO), an endocrine disruptor is “a chemical substance of natural or synthetic origin that is foreign to the body and can interfere with the functioning of the endocrine system, thereby inducing adverse effects on the body or its descendants
Endocrine disruptors can act on the hormonal system in different ways:
-by imitating or by mimicking the action of a natural hormone and thus causing the response due to this hormone.
-by blocking, by preventing a hormone from attaching to its receptor and thus impeding the transmission of the hormonal signal.
– by disrupting the production/degradation, or regulation of hormones or their receptors.
Because Ozalys was designed for women affected by breast cancer, our research focuses on the endocrine system. We are therefore careful not to introduce chemical or natural ingredients that behave like hormones into our formulas.
We also pay special attention to our packaging by using eco-responsible packaging, which protects the formulas and avoids migration of plasticizers so that you can use our range of care in complete safety and serenity.
HELP WOMEN TO LIVE WHILE UNDER HORMONAL THERAPY
According to the CANTO study, which aims to improve the quality of life of women affected by breast cancer (video link canto study https://youtu.be/Y0cQmFOc79A), one in six women stop their hormone therapy treatment one year after starting it.
Hormone therapy remains a key element in the therapeutic approach to hormone-dependent breast cancer, but how can we live with this treatment on a daily basis?
Dare to talk about it
Recognizing and adequately managing your adverse events is important to enable you to continue your treatment, which is why it is essential that you share your difficulties with your health care team.
Sport and a balanced diet can help reduce joint pain and regulate weight gain.
Hot flashes, which often appear after chemotherapy, are increased with hormone therapy, but can be reduced with complementary treatments such as alternative medicine. The Serelys, a hormone-free pollen-based product, also gives good results (60% reduction in symptoms in two months).
Hormone therapy can also sometimes lead to psychological discomfort and mood disorders. If this is the case, psychological support is available at all stages of the management of your illness. The administration of an antidepressant may sometimes
be necessary, but BEWARE certain molecules may be contraindicated with your treatment, so it is important to discuss this with your health care team.
Innovative techniques not widely used
Vaginal dryness, a frequent problem in women under hormone therapy but also in menopausal women, leads to sometimes very intense pain and ends up discouraging couples: it remains difficult to maintain a positive libido when each sexual intercourse results in an absence of pleasure or even pain sometimes at the borderline of bearable.
The solutions classically used during menopause are banned in the case of breast cancer and the solutions proposed to preserve women’s intimacy are both generally ineffective and not reimbursed. However, there are new strategies, such as vulvovaginal regeneration with hyaluronic acid injections or vaginal lasers, but these methods are not widespread and are not reimbursed by health insurance.
The vaginal laser is revolutionizing the sexuality of women who have had breast cancer (and all those who at menopause cannot or do not want to take hormones).
The vaginal laser : the explanations of Doctor David Elia , Gynecologist
The Vaginal Laser is an innovative treatment for vaginal dryness. 
The procedure is designed to treat vaginal atrophy, which is the main symptom of the disappearance of estrogenic hormones, with laser treatment. This is a set of symptoms such as vaginal dryness, irritation and especially pain during sexual
intercourse which in some cases ends up making sexuality impossible. In addition, the bladder and its evacuating canal – the urethra – also often suffer from hormonal deficiency: recurrent cystitis, urinary leakage with effort or impulses (or both) appear or increase.
You are therefore lying down in the gynecological position. A specific speculum is gently introduced to the bottom of the vagina, then the laser applicator is introduced inside the speculum. The actual treatment begins with the gradual removal of the applicator, the laser radiation then sweeping the vaginal mucosa for a few seconds.
A session consists of three successive treatment phases and lasts approximately 10-20 minutes. The ideal protocol consists of three sessions 4-6 weeks apart.
This laser procedure does not require any anesthesia and is performed in the doctor’s office on an outpatient basis because the sensations perceived are not or only slightly painful. The procedure is performed without incision, bleeding or sutures and does not require any pre- or post-operative care or medication.
Side effects are rare, but if they are present they are generally limited to a few uncomfortable and short-lived inflammatory sensations. Serious side effects have not been described to date, even though these procedures have been performed worldwide for at least 8 years.
In the vast majority of cases, the treatment allows a significant improvement of all the symptoms of vaginal atrophy, in particular vaginal dryness and pain, sometimes as early as the first session. The results are usually long-lasting, at least 18 to 24 months, but often longer. If necessary, one or two new sessions can then be offered successfully. Sexuality is again as often as possible satisfying and pain-free and those who were no longer sexually active can have sex again. Urinary symptoms (bladder weakness) usually improve or disappear.
Still not very widespread in France, unlike other countries, vaginal laser is not covered by the Health Insurance and the cost of the sessions is around 350 to 450€ depending on the private structures. Recently, some gynecologic and obstetrical hospital departments have begun to equip themselves with machines, which should make it easier to access this technology financially in the future
TO CONCLUDE
The Fighting Lady’s journey does not stop after treatment and daily life is sometimes difficult: irreversible after-effects, fear of recurrence, side effects of hormone therapy.
In this month of awareness and prevention in the fight against breast cancer, it seems to me that it is also important to raise awareness about post-cancer and the prevention of recurrence.
Because life is precious, because you are precious, Ozalys accompanies you during the illness, but also afterwards to help you (re)-build your future in complete serenity.

